Discover the best physiotherapy treatments for osteoarthritis in 2025! Learn how to reduce joint pain, improve mobility, and prevent surgery with expert-recommended exercises and therapies. Read now!

Osteoarthritis: Causes, Symptoms, and Physiotherapy Treatment.
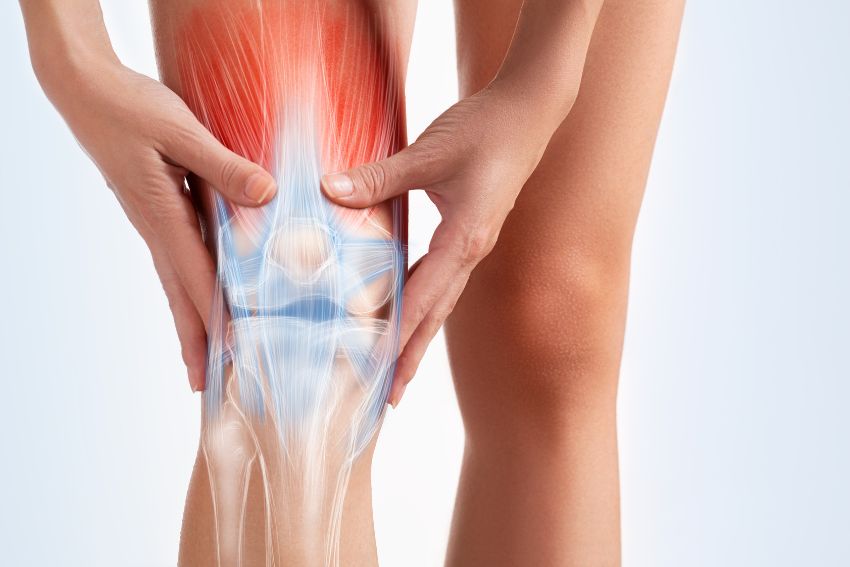
Osteoarthritis (OA) is the most common form of arthritis, affecting millions of people worldwide. It is a degenerative joint disease that occurs when the protective cartilage in joints wears down over time, leading to pain, stiffness, and reduced mobility. While it can affect any joint, OA is most commonly seen in the knees, hips, hands, and spine. Physiotherapy plays a crucial role in managing osteoarthritis, helping patients reduce pain, improve mobility, and enhance their quality of life.
In this blog, we will explore the causes, symptoms, and physiotherapy treatments for osteoarthritis
What Causes Osteoarthritis ?
Osteoarthritis develops when the cartilage in the joints gradually wears away, leading to bone-on-bone friction. Several factors contribute to its progression, including:
- Aging – The risk of OA increases with age due to natural wear and tear on the joints.
- Joint Injuries – Previous injuries, such as fractures or ligament damage, can increase the likelihood of OA.
- Obesity – Excess weight puts additional stress on weight-bearing joints like the knees and hips.
- Genetics – Family history plays a role, as some people inherit a tendency to develop OA.
- Repetitive Stress on Joints – Jobs or activities that involve repetitive motion can contribute to cartilage breakdown.
- Muscle Weakness – Weak muscles around a joint can lead to instability and increased wear on the cartilage.
Common Symptoms of Osteoarthritis
Osteoarthritis symptoms develop gradually and worsen over time. The most common symptoms include: Joint pain – Especially during or after movement.
- Stiffness – Most noticeable in the morning or after periods of inactivity.
- Swelling – Due to inflammation in the joint.
- Reduced flexibility – Difficulty moving the joint through its full range of motion.
- Grinding sensation – A feeling of bones rubbing against each other (crepitus).
- How Physiotherapy Helps in Osteoarthritis Physiotherapy is one of the most effective non-surgical treatments for osteoarthritis.
- A structured physiotherapy program can help reduce pain, improve mobility, and strengthen muscles around the affected joints.
Physiotherapy Techniques for Osteoarthritis
- Exercise Therapy Strengthening exercises to support the joint. Low-impact activities like swimming and cycling to maintain mobility. Stretching exercises to improve flexibility and reduce stiffness.
- Manual Therapy Hands-on techniques – joint mobilization to improve movement. Soft tissue massage to relieve muscle tension.
- Electrotherapy- Ultrasound therapy to reduce inflammation. TENS (Transcutaneous Electrical Nerve Stimulation) for pain relief.
- Hydrotherapy Water-based exercises help reduce joint stress while improving strength and movement.
- Posture and Gait Training Correcting posture and walking patterns to reduce joint stress.
- Education and Lifestyle Modifications Advice on weight management to reduce joint load. Guidance on using assistive devices like braces or orthotics.
Here are some simple exercises that can be done at home:
- Quadriceps Strengthening (Straight Leg Raise) – Helps support the knee joint.
- Heel Slides – Improves knee flexibility.
- Glute Bridges – Strengthens hip and lower back muscles.
- Ankle Pumps – Promotes blood circulation and joint mobility.
- Seated Knee Extension – Helps maintain knee range of motion.
Conclusion
Osteoarthritis is a progressive condition, but with proper management, it is possible to reduce pain and maintain an active lifestyle. Physiotherapy plays a vital role in strengthening muscles, improving joint function, and preventing further degeneration. If you or a loved one is struggling with osteoarthritis, consult a physiotherapist for a personalized treatment plan. By staying active, maintaining a healthy weight, and following a structured physiotherapy routine, you can manage osteoarthritis effectively and improve your overall quality of life.
FAQs About Osteoarthritis & Physiotherapy.
No, but with physiotherapy and lifestyle changes, you can manage symptoms and prevent worsening.
Yes! Walking is a low-impact exercise that keeps joints mobile and strengthens muscles.
Yes! Physiotherapy can delay or even prevent the need for joint replacement surgery by improving joint function.
Eat anti-inflammatory foods like salmon, turmeric, nuts, and leafy greens to support joint health.